Effectiveness of seasonal malaria chemoprevention in three regions ... - Malaria Journal
Study type and setting
The study examined data relative to children aged 3–59 months in three regions of Togo (Savanes, Kara, and Centrale) who received SMC according to the WHO recommendation of March 2012 [3]. These data were prospectively collected by the NMCP during the seasons of heavy rainfall over a maximum of four consecutive months (or rounds) per year (July–October) between 2013 and 2020.
The study area of 33,525 km2 (nearly 60% of Togo) is surrounded by Burkina Faso, Benin, Ghana, and Plateaux Region of Togo (Fig. 1). It includes three out of the six Regions of Togo, which corresponds to 16 health districts out of 44 and 324 health centers out of 987 in the whole of Togo. In 2019, the study area was home to nearly 2,829,887 people; i.e., nearly 30% of the Togolese population.
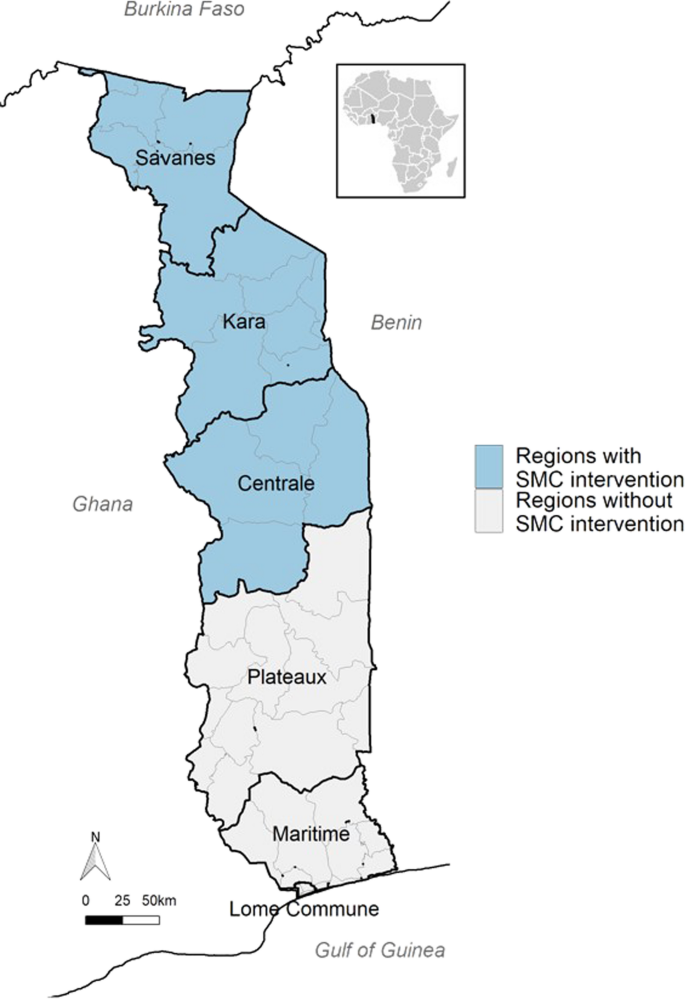
Seasonal malaria chemoprevention coverage area in Togo from 2013 to 2020 (source: National Malaria Control Programme)
From a climatic point of view, the study area is characterized by two seasons: a dry season from November to May and a rainy season from June to October with heavy rainfall between July and September. It is during the latter period that upsurges in malaria cases are seen and that SMC is administered.
Administration of SMC
Usually, a SMC campaign includes a maximum of four treatment rounds over four consecutive months. During each round, SMC is administered by hired community health workers (CHWs) who use two community approaches: (i) a 'door-to-door' approach by pairs of CHWs who visit households to identify children under five and administer the drugs; and (ii) a 'fixed-post' approach in health facilities to treat target children absent from home at the time of the CHWs' visit.
A treatment round consists in administering one dose of sulfadoxine-pyrimethamine (SP) and three doses of amodiaquine (AQ) over three days. SP and the first dose of AQ are given under the supervision of a CHW; the other doses of AQ are given on the next two days by a parent or a guardian.
Before their visits to the households, the CHWs receive specific training. Besides, the NMCP ensures that SMC beneficiaries understand the objectives of the treatment. This is usually done through awareness meetings with local leaders and dissemination of messages through various public media. During an SMC campaign, the supervision is generally provided by the managers of the health facilities, the districts, the Regions, and the NMPC.
Data collection
Sociodemographic data, administrative follow-up data, and information on adverse events were collected by 5787 CHWs from tools such as SMC cards, tally sheets, SMC treatment records, supervision forms, and adverse event count sheets. The CHWs had to report on specific sheets all adverse events occurring after treatment administration. These data were then compiled and validated by 324 health facility managers and sent to the 16 district managers. At the district level, these data were validated and transmitted to the three directors of the target Regions then to the NMCP. To improve the quality of those data and estimate the treatment coverage, the NMCP carried out community surveys at the end of each round.
Operational definitions
Malaria prevalence is the number of children with malaria (children with positive 'rapid diagnostic test' (RDT) plus children already treated for malaria) divided by the number of children identified in the eligible age range.
SMC coverage is the ratio of the number of children aged 3–59 months who received all SMC doses per round, district, or region to the number of eligible children identified per round, district, or region, respectively. Previously, expected numbers of children aged 3–59 months and eligible for a SMC campaign within a given region were provided by a statistics department supervised by the Togolese Ministry of Health and actual numbers of eligible children at implementation of each SMC round (thus, year) was obtained by the CHWs.
The effectiveness of a SMC campaign was defined as the percent reduction in malaria cases in each of the two or three last months of a campaign in comparison with the first month. Precisely, over the first year of SMC, a random sample of children who had received a first round underwent parasitemia (RDT) tests at the times of administration of the second, third, and fourth round to determine the proportion of infected children one month after the end of a year's SMC. This survey included only children whose caregivers confirmed the absence of consumption of other antimalarial drugs over each month following each round. The same survey was repeated in each of the following years. The yearly effectiveness was defined as the percent reduction in malaria cases for each year between 2017 and 2020, in comparison with year 2016. The numbers of malaria cases were obtained via health facilities and CHWs only (no external sources including pharmacies, NGOs), the proof being a positive RDT or a thick-blood-film test.
A SMC-related adverse event is any unexpected reaction in a child who received SMC treatment: vomiting, skin reactions (itching, hives), abdominal pain, somnolence, or jaundice. In Togo, cases of adverse events in children less than five are usually reported by the CHWs when administering the next round. In case an adverse event occurred soon after drug administration, the caregiver was asked either to inform the CHW (who generally lives in the same area) or visit the nearest health facility where the event is then reported on a specific sheet. Later, all adverse events are collected centrally for statistical purposes.
Statistical analysis
The prevalence of observed malaria cases in children was modeled using a logistic mixed regression model. Separate fixed effects for 'year' (reference year: 2016) and 'round' (reference round: first round of a campaign) were estimated using indicator variables and expressed as Odds Ratios (ORs). 'Year' and 'round' effects were entered as random effects and assumed to vary randomly according to the Region, the district, and the health facility. Effectiveness was calculated as 1 − (ORyear i, round j) with year 2016 and 1st round as references. This can be interpreted as the percent reduction of malaria prevalence. A second model was built including years 2013 to 2020.
The analyses used package lme4 and function glmer in R software (R Core Team, 2017; R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Ethics and regulations
This study was approved in 2017 by the Ministry of Health and Public Hygiene of Togo (Memorandum No. 280/17/SPS/CAB/SG/DGPIS/DPP/DER). The data collected, compiled, and stored by the NMCP did not require obtaining informed consents.
Comments
Post a Comment